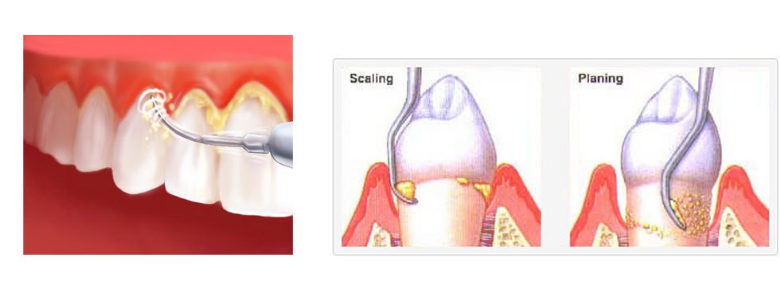
Tooth Scaling and Root Planing
Root exfoliation and planning is actually a thorough tooth cleaning procedure that is ideal in the early stages of periodontists. During this time, the individual’s teeth may develop pockets of abnormal spaces between the teeth. As these pockets enlarge, the teeth will separate from the gums and eventually fall out.
Excess bacteria on teeth can also be accidentally ingested and make a person sick. This situation is very serious for people with heart-related conditions because bacteria can get into the bloodstream and cause inflammation in the chambers of the heart.
Scaling and root planing are generally administered as a single treatment under local anesthesia unless there is significant tooth damage. During the “scaling” portion of the procedure, the dentist uses mechanical aids to remove excess bacteria from the teeth. The bacteria can be in the form of plaque, tartar, or cavities.
The “brushing” part of the procedure involves cleaning below the gum level. Because bacteria may not be visible, the dentist looks for rough surfaces and uses a handpiece to remove any dirt or bacteria. There are two common types of hand instruments: an ultrasonic instrument or a scraper. Dental patients tend to prefer the ultrasound instrument because it causes less discomfort.
Suitable candidates
To determine whether a person’s periodontal disease is appropriate for Tooth scaling and root planing, dentists use a guide from the American Dental Association (ADA). According to the ADA, gum disease that extends 3-6 millimeters below the gum line is suitable for scraping and root planning. Gum disease deeper than this amount will likely require surgery.
After the procedure
Because scaling and root planning involve the dentist working on sensitive areas of the teeth and gums, people may experience some soreness, soreness, and minor bleeding after the procedure. The individual may also notice a temporary sensitivity to hot or cold drinks.
In most cases, over-the-counter medications are sufficient to relieve symptoms. The dentist should be contacted if it persists for an extended period of time.
Recently I looked at “official” information about gum disease and gingivitis. One of the sites suggested that gum disease was the result of poor brushing and flossing. I think this is potentially a false and potentially dangerous statement, as it can lead people to believe that they are free from gum disease if they brush and floss regularly.
The Mayo Clinic website estimates that about 80% of Americans suffer from gum disease. Another source states that between 75% and 95% of the population is affected. If someone were to suggest that 80% of Americans don’t brush or floss properly, my answer would be that while many Americans have this problem, it’s not very likely that 80% will. I think it’s more plausible to conclude that brushing and flossing are generally not enough to prevent gum disease.
In my own example, I brushed and flossed more often than the average person and still developed it. I visited a dental hygienist’s website and she wrote that regular brushing and flossing was not enough to prevent gum disease. With decades of experience to back it up, I think your opinion is qualified.
Age will probably not be a determining factor either. I’ve noticed that even some very young adults have red or purplish swollen gums. This is pathetic. I’m sure the dental office could create great and effective new home treatments that would help the vast majority of adults prevent or beat gum disease. If you are a dentist reading this, I hope you will personally take up the banner of gum disease prevention and advocate for this cause.
He didn’t really understand what gum disease was and didn’t think he actually had it. I thought it was normal to have some bleeding while brushing and flossing. Later I discovered that this idea was wrong. Bleeding while brushing and flossing are signs of gum disease. If your gums bleed while brushing or flossing, even a little, it is NOT normal.
A family member told me that he had undergone the Tooth descaling and root planing treatment and that the results were not as good and that he felt that his gums were worse than before the treatment. I chose not to undergo the treatment and decided to do my own research on it. What I found was quite alarming. The main cause of tooth loss is gum disease. More people have it or its precursor, gingivitis, than you might reasonably suspect.
Then I came across a few things that, together, worked to improve the health of my gums. What I did I created a website called ‘Gingivitis Killer’ to educate people about the combination of tools I used to halt the progression of gum disease and prevent it from escalating again. However, if you have or suspect you have gum disease or gingivitis, see your dentist immediately for diagnosis and treatment.



